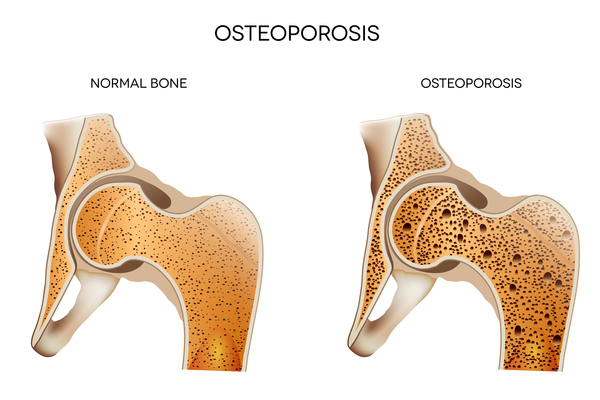
Meet Jim, a 29-year-old warrior battling systemic lupus erythematosus. For the past decade, she’s been on a rollercoaster ride with prednisone, a corticosteroid that’s both her ally and her adversary. After five years of treatment, she thought she was in the clear. But three years ago, her back started to ache, and it wasn’t just a passing discomfort. Her spine was crumbling, and she found herself 2 cm shorter. A bone density test revealed the unsettling truth: osteoporosis, with a compression fracture in her first lumbar vertebra.
“I pop calcium pills like candy, how did this happen?” Jim asked her doctor, bewildered. To understand her plight, let’s dive into the world of glucocorticoid-induced osteoporosis.
Is Glucocorticoid-Induced Osteoporosis Common?
Back in 1950, British pharmacologists Hench and Kendall struck gold when they discovered glucocorticoids and their miraculous effects on rheumatological diseases. Fast forward to today, and we have a plethora of corticosteroids like prednisone, prednisolone, methylprednisolone, and dexamethasone, all heroes in the fight against inflammation and immune disorders. But like any double-edged sword, these drugs come with a hidden cost: stealthy bone erosion.
In China, a staggering 90% of rheumatology patients on corticosteroids experience bone loss, with 41.4% developing osteoporosis. In the West, up to 40% of long-term corticosteroid users suffer fractures, with the risk escalating with higher doses and longer durations. So, Jim, osteoporosis and fractures are more common than you think among corticosteroid users. Keep your guard up!
Why Do Glucocorticoids Cause Osteoporosis?
Corticosteroids are like the ultimate party crashers for your bones. They mess with osteoblasts (bone builders), osteoclasts (bone breakers), and osteocytes (bone cells). On one hand, they stunt osteoblast growth, slowing down bone formation. On the other, they boost osteoclast activity, accelerating bone breakdown. They even trigger osteocyte apoptosis, thinning your bone cell population. Plus, they hamper calcium absorption in your gut and kidneys, dampen your gonadal function, and shrink your muscle mass, all of which indirectly weaken your bones.
What Makes Glucocorticoid-Induced Osteoporosis Unique?
- Duration and Dose Matter: Bone density takes the biggest hit in the first year of corticosteroid use, dropping by 12-20%. After that, it continues to decline by about 3% annually. The higher the dose, the steeper the decline, whether it’s a daily or cumulative dose.
- Fracture Frenzy: Long-term corticosteroid users are more prone to fractures, especially vertebral fractures.
- Partial Recovery Post-Stop: Bone density can partially rebound six months after stopping corticosteroids, but if you’ve lost too much, it’s a lost cause. Vertebral deformities and back pain may persist.
- Bone Density Isn’t Everything: Corticosteroids degrade bone quality, so even if your bone density looks okay, you’re still at risk for brittle fractures.
How to Treat Glucocorticoid-Induced Osteoporosis?
Many, like Jim, mistakenly believe that popping calcium pills is enough to ward off corticosteroid-induced osteoporosis. In China, only 4% of long-term corticosteroid users take osteoporosis drugs like bisphosphonates. In the West, it’s a mere 20%.
Here’s the reality: Anyone on corticosteroids for ≥3 months needs to consider osteoporosis prevention.
- Reduce the Dose: Work with your rheumatologist to minimize corticosteroid use by adding disease-modifying antirheumatic drugs (DMARDs).
- Assess the Risk: Your bone metabolism specialist will evaluate your fracture risk based on corticosteroid dose, duration, age, menopausal status, smoking, falls, and past fractures. Tools like FRAX will help categorize your risk.
- Low Risk? Lifestyle Changes: For low-risk cases, focus on a balanced diet, maintaining a healthy weight, quitting smoking, engaging in weight-bearing or resistance exercises, limiting alcohol, getting sunlight, and preventing falls. Supplement with 1000-1200 mg of elemental calcium and 600-800 IU of vitamin D daily.
- Moderate to High Risk? Add Medication: For higher risks, add osteoporosis drugs like bisphosphonates, teriparatide, denosumab, raloxifene, or calcitonin.

For Jim, the doctor recommended increasing dairy intake, moderate activity, avoiding heavy lifting, falls, and injuries. She started on 600 mg of elemental calcium and 800 IU of vitamin D3 daily, plus an annual infusion of zoledronic acid. Her back pain eased, and her height stabilized. She’ll continue regular check-ups and risk assessments.
In summary, corticosteroids are a double-edged sword. While they save lives, they also silently erode your bones. Stay vigilant, make lifestyle changes, and don’t shy away from medication if needed. Your bones will thank you!




Leave a Reply